The experiment is simple: Apply a layer of cells to the surface of a petri dish, then scratch a line through them, down the middle. In her lab at Bucknell University, Drexel triple alumna Olivia Boerman (BS ’17, MS ’18, PhD ’22) then exposes the dish to low-intensity ultrasonic waves.
Ten hours later, the dish exposed to the ultrasonic waves has a gap less than half the size of its untreated counterpart — evidence that Boerman can accelerate the movement of cells to fill voids in a way that mimics wounds and the healing process.
One day, ultrasound-based therapies may be able to spur endothelial cells like the ones she studies into rebuilding oxygen and nutrient pathways in tissue damaged by the many conditions that can choke off the blood supply, such as atherosclerosis and rheumatoid arthritis. Widely used as a diagnostic, ultrasound is less common as a treatment of injury and disease, but emerging research like Boerman’s promises intriguing therapeutic potential.
John Wild and John (Jack) Reid. Photo Credit: Eric Blackwell
“It’s remarkable to me that something as innocuous as sound waves would cause cells to move faster,” says Boerman, who joined Bucknell as assistant professor of biomedical engineering after completing three biomedical engineering degrees in Drexel’s School of Biomedical Engineering, Science and Health Systems (BIOMED).
For her, the sight of the shrinking, simulated wound has been another breadcrumb leading her deeper into a research question that began at Drexel. As a student, she saw clinical trial results of an ultrasound device developed by her mentor, Richard B. Beard Distinguished University Professor Peter A. Lewin. The results showed that venous ulcers caused by poor blood circulation healed faster after being exposed to four 15-minute treatments with ultrasound. Hooked, Boerman went on to study the topic for her doctorate under the guidance of Lewin and Kara Spiller, URBN Professor of Biomedical Innovation.
Through such projects, biomedical engineering faculty and alumni at Drexel are continuing a legacy of ultrasound innovations at the University that dates back roughly four decades to around the time a pioneer of the field, John (Jack) M. Reid, joined the faculty.
Reid, who passed away last year at the age of 97, was a globally recognized scholar and renowned engineer. His mechanical prowess out of college enabled him to translate military ultrasound technology used to spot submarines (SONAR) into a medical mainstay, an achievement that preceded a career-long dedication to building devices that help doctors detect hidden conditions using non-invasive ultrasound.
His arrival at Drexel helped to precipitate an institutional focus on this versatile technology that continues to this day, carried on through researchers and their protégés.
In the generations since medical ultrasound first emerged in the early half of the 20th century, it has touched the lives of nearly everyone. Widespread ultrasound-based imaging offers a glimpse of babies still in the womb, hidden injuries, and tumors lying in wait, among other things. Medicine also employs it to blast kidney stones and cancer, remove cataracts, and heal bone fractures. Newer research is exploring its use in treating addiction, even, and it has the potential do much more as a therapy.
“I really think that ultrasound technology is absolutely applicable to everything that you see in health care,” Lewin says. “The next couple of decades will show its superiority.”
From Radical Idea to Reality
The frequency of sound waves is determined by how many cycles they complete over a second as they travel through air or water. Human hearing can detect sound waves that cycle between 20 and 20,000 times per second. Increase the frequency to more than 20,000 a second — ultrasound — and they become inaudible yet capable of a kind of sight, giving doctors a shadowy topographical view of the body’s interior, without a single incision.
Ultrasound works because when sound waves strike an object, some are absorbed, and some reflect back toward the source. The reflected waves produce an echo, which certain animals, notably bats and marine mammals, have long harnessed to navigate their environments.
During World War I, submarine warfare inspired scientists to exploit soundwave echoes for detecting submerged enemy vessels. Decades later, the surgeon John Wild experimented with using them to examine internal injuries noninvasively. In 1950, he recruited Reid, a former Navy electronics technician fresh out of college, to adapt SONOR technology for medical diagnostic equipment.
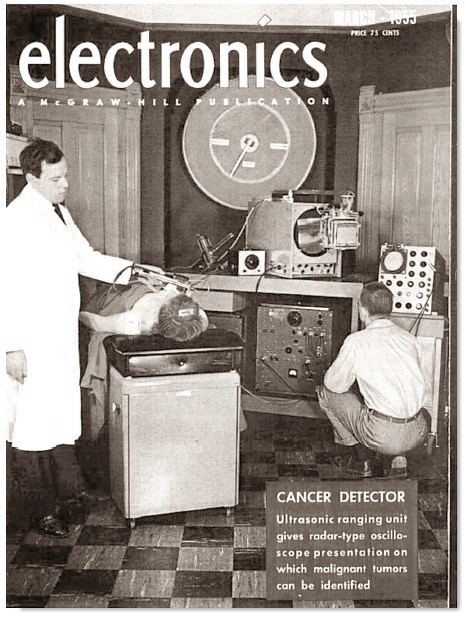
Within a few months of starting his new job in his boss’s Minnesota basement, Reid had built a prototype, which he and Wild tested on a cube of beef. In 1952, they published the first 2D ultrasound images of a tumor, depicted as a distinctive mass within the left thigh muscle of a patient. Wild and Reid knew they were onto something, writing that they envisioned “[t]he immediate application of echography [ultrasound] to the detection of tumors in accessible sites in the living intact human organism.”
At first, the scientific community responded less enthusiastically to the blurry black-and-white sonograms the pair produced.
“They didn’t understand what they’re looking at,” Lewin says of radiologists at the time. “And they said, ‘Oh, this will never work.’”
But Reid and Wild’s results suggested otherwise. They recruited breast cancer patients as test subjects, correctly identifying 31 out of 35 malignancies. In 1955, their work was featured on the cover of Electronics magazine.
Reid marked more milestones in his field over the decades that followed. At the University of Pennsylvania, he worked with Claude Joyner, later viewed as one of the early pioneers of echocardiography, to build an ultrasound machine adapted for the heart. The first such machine in the United States, it picked up the motion of the organ’s valves, improving heart condition diagnoses.
Reid realized, however, that to truly see what was happening within this organ, he needed to be able to monitor blood flow. So, he moved on to working with Doppler ultrasound, which detects the movement of blood cells. The resulting technology has made it possible to noninvasively detect and diagnose atherosclerosis, a major contributor to heart disease deaths.
In 1981, he was appointed Drexel’s first Calhoun Chair of Biomedical Engineering at a fête where figures from the National Science Foundation and the National Institute of Health gave introductory remarks.
A Legacy of Leadership
While at Drexel, Reid’s research focus shifted from building equipment to studying the mathematics required to generate sonograms. But he is most remembered by colleagues for the impact of his leadership on students, colleagues and the growth of the institution.
“He put Drexel on the map in the following years by attracting high-quality undergraduate and graduate students,” Lewin says. “And he indisputably enhanced BIOMED’s reputation.”
Nearly a decade into his tenure, Reid led a Drexel team of researchers to obtain a highly prestigious grant from the National Institutes of Health. By Lewin’s estimates, that grant was a substantial portion of the nearly $18 million in funding that Reid brought to Drexel over the years.
The grant fueled projects aimed at enhancing ultrasound’s ability to detect and describe tumors, an effort that would last more than a decade and generate dozens of publications.
Lewin, who arrived at Drexel as a visiting professor at about the same time as Reid, ran one of the grant projects aimed at developing a new, versatile class of low-frequency ultrasound probes. And Reid encouraged another Drexel newcomer, Margaret Wheatley (who today holds the John M. Reid Professorship within BIOMED), to investigate chemically developing and testing bubbles. Together the interrelated projects allowed faculty members to experiment with ultrasound from many different angles, and it laid the groundwork for the eventual founding of BIOMED.
Prior to 1997, Reid and his colleagues operated within a unit known as the Biomedical Engineering and Science Institute (BMESI), BIOMED’s predecessor. That year, a group of seven faculty members — led by founding director Banu Onaral and including Lewin and Wheatley — persuaded then-President Constantine Papadakis to create a standalone school of biomedical engineering where experts in chemistry, biology, physics, medicine and engineering could explore interdisciplinary biomedical research together.
The venture came at great professional risk: Papadakis challenged the professors to sacrifice their tenure, telling them, “You submit your tenure, and if three years from now, you still exist and have the first graduate, you’ll get back your tenure.” And so they did.
As an institution, BIOMED was ahead of its time, one of the region’s earliest institutions to focus on cutting-edge medical engineering. Citing his mentorship, Onaral credits Reid’s influence on the group’s strategic thinking when transforming BMESI into a first-in-class interdisciplinary undergraduate program.
“Professor Reid’s academic vision, his pioneering research in biomedical ultrasound, his commitment to innovation, and more importantly, his generosity of spirit focused on the learner and the junior faculty are imprinted in our institutional DNA,” she says.
Reid was an invaluable sounding board to other researchers, Lewin says. “It’s very difficult to work in this particular area if you don’t have somebody to share the ideas with and to criticize what you’re doing in a constructive way,” he says. “Reid had this intuition which would say, ‘Oh, yes, that would work and that won’t.”
Nowadays, Lewin is focused on using ultrasound to heal chronic wounds. While echoes provide the basis for imaging, tissue also absorbs energy from ultrasonic waves that can alter it and even, potentially, encourage healing. For reasons that aren’t fully understood, low-frequency ultrasound appears to aid healing in recalcitrant ulcers, which often affect diabetics because the condition prevents blood flow necessary for wound healing. Working with College of Medicine doctor Michael Weingarten, MD, Lewin is developing a light, inexpensive, patch-like ultrasound device that patients can wear at home. They envision that it could one day be integrated into a compression sock.
Boerman came to Drexel through the Liberty Scholars Program, which supports students with financial need. Without the full scholarship it provided, “I probably would be doing nails in my mom’s nail salon at the moment,” she says.
With her advisers Lewin and Spiller, she focused on macrophages, immune cells that contribute to inflammation, in tissue samples from patients’ ulcers. While initially protective, the inflammatory response remains elevated for too long in these wounds, interfering with healing. Ultrasound treatment, she found, decreased the macrophages’ inflammatory activity — one potential explanation for how it may benefit these injuries.
She recognized the technology’s larger potential. “At low intensities, it has no adverse effects on the body,” Boerman says. “It really is encouraging natural healing in a way the body won’t reject as foreign.”
But so far, ultrasound’s ability to alter the behavior of cells remains untapped.
In 2022, Boerman joined the faculty at Bucknell, a private liberal arts college in central Pennsylvania, where she has continued to study these mysterious effects. Drawing on her training at BIOMED, she wrote a proposal for and, in March, received a National Science Foundation award that will allow her to take the next step in her research. In real-world healing, macrophages and endothelial cells interact within the 3D structure of human tissue. With this funding, she plans to apply both types of cells to scaffolds of collagen, a protein throughout the body, and investigate how ultrasound influences their behavior.
“If we can crack this code of understanding what ultrasound does on a biological level, I really think it is the future of healing,” she says.
Making Waves and Bubbles
Elsewhere in the halls of Drexel’s School of Biomedical Engineering, Science and Health Systems, Reid’s former colleague, John M. Reid Professor Wheatley, is carrying on the school’s tradition of mentorship with her own protégés.
One of her cutting-edge projects involves injecting miniscule gas bubbles by needle into a patient’s vein.
Gas bubbles injected into a patient work on the same principle that allows fishermen to spot schools of fish with sonar. Fish control their position in the water with air-filled sacs called swim bladders. The pocket of air within the organ reflects fish-finding ultrasonic waves much more strongly than the surrounding water, just as injected gas bubbles reflect medical ultrasound.
When she arrived at Drexel in 1987, she specialized in packaging drugs for delivery within the body. Not long afterward, the head of ultrasound at Thomas Jefferson University in Philadelphia at the time, Barry Goldberg, MD, introduced her to what was then a new line of research: enhancing the visibility of a tissue or structure within an ultrasound image using microbubbles. He gave her some papers documenting earlier studies and a small grant to develop her own version of this experimental contrast agent.
Wheatley recalls him asking at their first meeting, “Can you micro-encapsulate the bubbles, or surround them with a shell? Oh, and by the way, they have to be less than eight microns [millionths of a meter] in size.” That, it turns out, is not an easy task, she says.
But she succeeded, and so helped usher microbubbles into medicine, continuing BIOMED’s legacy of innovation. The FDA has since approved these tiny, gas-filled structures for examining the heart and detecting liver tumors and urinary reflux. The bubbles have also proven remarkably versatile, opening the door to many other applications.
“We put drugs into the shell, we put different gasses inside, we attach molecules to the outside that will recognize the surface of tumor cells,” Wheatley says of experiments in her lab and others.
“Things are moving so fast now; I often feel that I was born 20 years too early.”
In one ongoing project, she and her former student, now an associate professor at Thomas Jefferson University, are seeking to improve radiation therapy for cancer with oxygen-filled bubbles encapsulated by shells containing an experimental drug. A common treatment for cancer, radiation is more effective in the presence of oxygen.
As with tissue, microbubbles don’t just reflect ultrasonic signals. The energy from the ultrasound can also cause them to expand and contract, even burst — at just the right time and in just the right place, on a scale of millimeters. Once the bubbles have infiltrated a tumor, the team hits them with targeted ultrasound, popping them. They release oxygen and the medication, rendering the malignancy more vulnerable to radiation.
While Wheatley and Eisenbrey have yet to test their oxygen-based approach in patients, other similar applications for microbubbles are now in clinical trials. Eisenbrey is testing the ultrasound-microbubble combo’s potential against malignancies of the liver, bile duct and pancreas. So far, the data overall suggest that this approach can increase the cancers’ response to radiation and chemotherapy, improving patient survival.
“There’s a huge potential, and I think we’re not that far away from reaching it,” Eisenbrey says.
Experimental ultrasound therapies show promise in another field too — the treatment of infections. Another of Wheatley’s mentees, Lauren Delaney, ’11 MS, ’16 PhD, now a research assistant professor at Jefferson, is working on an ultrasound-based approach to protecting patients in the aftermath of spinal fusion surgery.
Normally, surgeons apply powerful antibiotics after implanting a bone graft to stabilize the spinal column. Even so, bacterial colonies can adhere to the implant and create havoc for the patient. Delaney has designed a bead-like cartridge that clips onto titanium rods in the implant. When exposed to ultrasound, the device releases an antibiotic, what she terms a “second wave” of protection, that could be activated three to five days after surgery.
She also hopes to follow up on other studies suggesting that bursting microbubbles can augment the effects of antibiotics and other measures for treating knee infections, like those that can follow joint replacements.
“If we can show that microbubble rupture increases our ability to treat infections, then we could apply it more broadly,” she says, noting that battlefield wounds and aggressive skin and soft tissue infections are among those conditions that could benefit.
She’s found further inspiration in ultrasound research on the brain. By activating microbubbles, scientists have succeeded in temporarily opening the blood-brain barrier, an accomplishment that could make it easier to get drugs into the brain. Other studies are exploring microbubbles and ultrasound as a potential means for treating Alzheimer’s disease.
She dreams of one day experimenting with cranial ultrasound, “but that’s down the line,” she says.
A World of Possibility
Before he passed away, Reid had the chance to witness the field he helped establish evolve dramatically from the first fuzzy sonograms he produced. At the end of a presentation he compiled for use in 2003, three years after being elected an honorary member of the World Federation for Ultrasound in Medicine and Biology, he offered a few thoughts on where the field could go, and left the possibilities wide open.
“Predictions are the tricky part!” Reid wrote. “[B]ut desires are more certain.”